High-pressure balloon dilatation in children: our results in 30 patients with POM and the implications of the cystoscopic evaluation
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
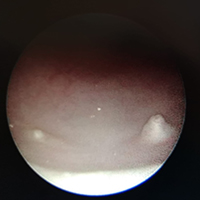
Primary Obstructive Megaureter (POM) is a common cause of hydronephrosis in children with spontaneous resolution in most cases. High-Pressure Balloon Dilatation (HPBD) has been proposed as a minimally invasive procedure for POM correction in selected patients. The aim of the paper is to review our experience with HPBD in patients with POM. We performed a retrospective study in a single Centre collecting data on patients’ demographics, diagnostic modalities, surgical details, results and follow-up. In particular, the endoscopic aspect of the orifice permitted the identification of 3 patterns: adynamic ureteral segment, stenotic ureteric ring and pseudoureterocelic orifice. We performed HPBD in 30 patients over 6 years. We had 23 patients with adynamic distal ureteral segment (type 1), 4 with stenotic ring (type 2) and 3 with ureterocelic orifice (type 3). In 3 patients (10%) the guidewire did not easily pass into the ureter requiring ureteral stenting or papillotomy. Post-operative course was uneventful. Five patients (3 pseudoureterocelic) required open surgery during follow-up. HPBD for the treatment of POM is a safe and feasible procedure and it can be a definitive treatment of POM. Complications are mainly due to double J stent and none of our patients had symptoms related to vescico-ureteral reflux. The aspect of the orifice, identified during cystoscopy, seems to correlate with the efficacy of the dilatation: type 1 and 2 are associated with good and excellent results respectively; type 3 do not permit dilatation in almost all cases requiring papillotomy. HPBD can be performed in selected patients of all paediatric ages as first therapeutic line. The presence of a pseudoureterocelic orifice or long stenosis might interfere with the ureteral stenting and seems associated with worse outcomes.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.