Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
GERD surgery in non-neurologic patients: Modified Laparoscopic Hill-Snow Repair is a valid alternative to Nissen fundoplication. Results of a 20 years of follow-up
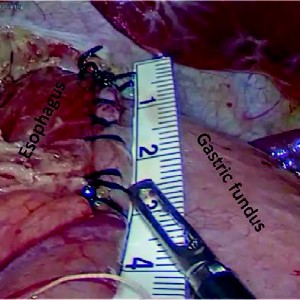
Nowadays laparoscopic Nissen fundoplication represents the gold standard in surgical treatment of complicated Gastro-Esophageal-Reflux Disease (GERD), above all in cerebral palsy patients. In non-neurological patients without gastrostomy Nissen fundoplication can create some problems (gas bloat syndrome, dysphagia). Laparoscopic Hill-Snow repair is an established surgical alternative, but it is reported only in adult population. We describe our modification of Hill-Snow technique and our experience in a large series of non-neurological children in order to report its effectiveness and applicability in pediatric patients affected by complicated GERD. Between 2000 and 2022, 319 children underwent surgical correction of gastro-esophageal reflux at our Department. All were affected by complicated gastro-esophageal reflux unresponsive to PPI (Proton Pump Inhibitors). 251 underwent laparoscopic Nissen fundoplication; 68 non-neurological patients underwent laparoscopic Hill-Snow repair. Of these 68 children 48 were males (71%) and 20 females (29%); median age was 5years (3 months-11 years). Weight range was 4-37kg.
52 patients (76.5%) presented the following symptoms: retrosternal pain, dysphagia, regurgitation, coughing, failure to thrive, persisting reflux esophagitis. 16 (23.5%) had chronic respiratory problems (aspiration, apneic-spells, dysphagia, coughing, choking, gagging). For 8 (11.8%) symptoms were expression of chronic recurrent gastric volvulus. All underwent modified-laparoscopic-Hill-Snow repair. Contrast study showed sliding hiatal hernia in 55 patients (81%), while endoscopy demonstrated 16 cases of histologically severe esophagitis (23.5%) and 52 of mild esophagitis (76.5%). No intraoperative/postoperative complications were recorded. 60patients had a complete follow-up (range 1-20 years). 60/68 patients were evaluated with barium-swallow-study at 6-12 months; 40/68 patients with upper-gastrointestinal-endoscopy at 12months. No relapse was reported. 50 patients (73.7%) were symptom-free. 18 (26.3%) referred occasional epigastric pain, associated with vomit in 2 cases. 64 (94.1%) referred ability to vomit; 4 temporary difficulty to swallow (average 30 days). All patients reported being able to burp. 3(4.5%) presented episodes of gas-air-bloat during the first 2 months with spontaneous resolution. No case of dumping syndrome was recorded. This technique’s modification yields excellent results in term of relapse and side effects at long-term follow-up. We reported the first and largest pediatric series in non-neurological children with encouraging results.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.