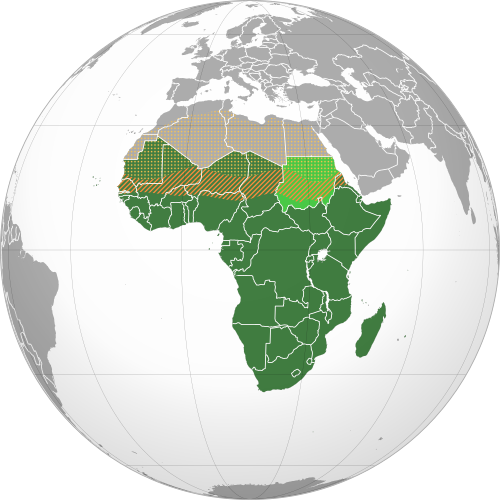
The hidden burden of Pediatric urology in Sub-Saharan Africa: an analysis of hospital admission data from three East African Health Centres
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
Specialist facilities for children are still unavailable in some Sub-Saharan African contexts. It is the case of pediatric urology, whose recent advances are still largely unshared. Prenatal diagnosis of urinary abnormalities (CAKUT) is largely unknown. Early recognition and referral of Undescended testis (UDT), Hypospadia, bladder exstrophy epispadias complex, ambiguous genitalia, stone disease, and tumours are uncommon in rural areas. Missed diagnosis is not uncommon and delayed management is associated with poor outcomes. We present a cross-sectional, descriptive study about the epidemiology of Pediatric urological admissions to three sub-Saharan East African Hospitals. All the urological cases between 0-18 years referred to three distinct East African Hospitals over 124 weeks were considered. Prevalence of different groups of diseases, age, and mode of presentation were reported. We found 351 cases (M/F 127/24) out of 2543 surgical referrals (13%). Seventy percent of cases were Hypospadias and UDT. Fifty percent of UDT were beyond 6, and most Hypospadias were between 4 and 7 yrs. CAKUT had a very low prevalence (4.84%), and about 50% of Wilms Tumours came too late to be resectable. In many African contexts, urology is still a tiny portion of the pediatric surgical workload compared to the 25% of European and American reports. There are also differences in the epidemiology of genitourinary conditions. A hidden burden of diseases may be presumed, remaining undiagnosed due to the shortage of specialist facilities.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.